The Temple is committed to supporting the development of a body of scientific research that can demonstrate the efficacy of Amazonian plant medicines and healing processes.
From 2015 to 2019, we hosted a landmark research project studying ayahuasca as a therapeutic tool in modern society with the International Center for Ethnobotanical Education, Research, and Service (ICEERS) and the Beckley Foundation.
Our collaboration studied the long-term effects of ayahuasca on quality of life, well-being, and health, with sub-sections on anxiety, depression, grief, and PTSD. The study is unprecedented and the preliminary results are highly significant. It also provided valuable feedback on Temple program satisfaction.
Results from participants who took part in clinical personality and psychopathology testing reveal empirically significant results immediately following the Temple’s healing programs and also after a long-term integration period.
Due to the quantity of data that has been generated by this study, researchers at ICEERS and Beckley Foundation expect to be publishing articles in five different peer-reviewed medical journals in 2020 and 2021, a significant addition to scientific literature and evidence on ayahuasca healing as a highly effective way to treat deep-rooted psychological and emotional conditions that cannot be treated by conventional pharmaceutical medication and practices.
Publications
1st published article:
González, D., Cantillo, J., Pérez, I. et al. Therapeutic Potential of Ayahuasca in Grief: a Prospective, Observational Study. Springer Journal of Psychopharmacology, Jan 14th 2020.
“This is the first study to prospectively assess the long-term effects of ayahuasca in participants grieving the death of a loved one. In this observational study, the primary result showed that the severity of grief significantly decreased after drinking ayahuasca, being maintained over 1 year of follow-up. This study offers preliminary findings in support of the long-term therapeutic potential of ayahuasca for bereavement.
A significant improvement in the severity of grief and the high effect size maintained over a year of follow-up are sufficiently encouraging to warrant further research. Furthermore, the assessment of experiential avoidance and decentering highlights the improvement of these mechanisms of change following drinking ayahuasca and their relation to grief improvement.”
2nd published article:
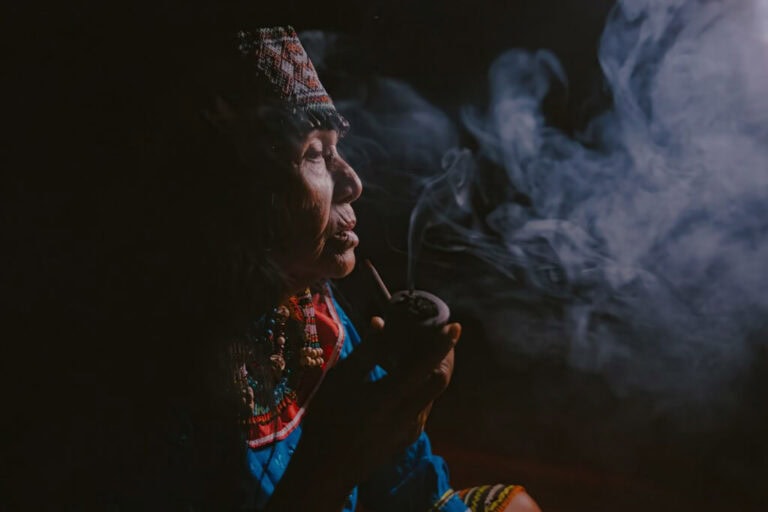
González, D., Cantillo, J., Pérez, I. et al. The Shipibo Ceremonial Use of Ayahuasca to Promote Well-Being: An Observational Study. Frontiers Journal of Pharmacology. May 5th 2021.
“In this prospective, observational non-controlled study, we examined the long-term impact that ayahuasca, used in a ceremonial Shipibo context, can have on the integral well-being of the individual. Participants who have completed the evaluations throughout the year show a significant increase in psychological well-being, subjective well-being, spiritual well-being, and quality of life after their stay in the retreat.
These outcomes are confirmed by the reports of most of the participants who affirmed sustained benefits on personal well-being over one year, followed by spiritual benefits. The subgroup analysis performed in a representative subsample allowed us to infer that the significant differences in outcomes are due to the effect of their stay at the center and not the passing of time.”